Thursday, November 26, 2020
Lupine Publishers: Happy Thanksgiving!!!
Wednesday, November 25, 2020
Lupine Publishers: Lupine Publishers | Information and Communication ...
Tuesday, November 24, 2020
Lupine Publishers: Lupine Publishers | Information and Communication ...
Monday, November 23, 2020
Lupine Publishers: Lupine Publishers | Allele Mining for the Reported...
Friday, November 20, 2020
Lupine Publishers| CeA & BNST: D2R &Impulsivity
Lupine Publishers| CeA & BNST: D2R &Impulsivity
Lupine Publishers| Neurology and Brain Disorders
Introduction
Impulsivity
Impulsivity is defined as a predisposition to performa with slight or no forethought or deliberation of the consequences and is a most important element of several psychiatric ailments [1]. It transpires in a various form, which can be branded as:
a) Choice Impulsivity: Acting to attain a less important instant reward against a superior late reward.
b) Impulsive Action: The incapability to prevent an initiated action.
c) Reflection Impulsivity: A deed lacking sufficient evaluation of information.
d) Attention Impulsivity: Diminished capacity to persevere a germane behaviour avoiding other distractions [2].
Impulsivity and addiction
The pathological trademark of addiction disorder is Impulsivity. It is principally thought that Addiction can be caused due to diminished inhibitory control [3]. Impulsivity is closely associated with drug dependence and abuse. The tendency to pick a subordinate, but instantaneous, reward over a significant outcome which occurs late. Addiction is nothing but the discrepancies in regulating the inhibitions due to disability to properly constrain actions or thoughts that lead to impetuous actions. There is a clear overlap amongst addiction and impulsivity, which leads to the conclusion that there is an overlapping neurobiological mechanism on which these processes depend on. Undeniably, it is suggested that the dopaminergic transmission and corticostriatal system is the communal neurobiological substrate for these behaviours. Addiction is demonstrated by various studies that display a noteworthy reduction in striatal dopamine transmission that is determined as pre-synaptic dopamine release and dopamine D2 receptor binding [2].
Amygdala
Amygdala is modest in dimensions, as it is includes many interrelated nuclei burrowed in the deeper parts of temporal lobe. BLA is the basolateral complex of the amygdala that is constitutes BM-basomedial, LA- lateral, BA- basal cell groups. principal neurons of BLA are glutamatergic and inhibitory interneuron. CeA is the central nucleus of amygdala which consists of CeL the lateral subdivision and CeM the medial subdivision. CeA neurons are principally GABAergic. the CeL projects to CeM. Intercalated cells are the primary source of inhibition is a group of interconnected GABAergic neurons, connecting the BLA and CeA [4].
CeA: Central Amygdala
Extended amygdala: The neurotransmission inside the intangible macrostructure in the basal forebrain is accredited to several long-standing emotional conflicts connected to alcohol abuse and addiction. The major constituents of the extended amygdala are the CeA, BNST (bed nucleus of stria terminalis, and NAc (nucleus accumbens) [5]. The inputs of extended amygdala include afferents from hippocampus, limbic cortices Basolateral Amygdala (BLA). They also demonstrate similarity in morphology and has overlapping and interconnected neural circuits. Whereas the primary outputs to various areas that produce behaviours associated with anxiety and fear such as lateral brain stem regions and hypothalamus. The extended amygdala constitutes the neurotransmitters connected with positive reinforcing effects of abusal of drugs and the key apparatuses of the brain stress systems connected to negative reinforcement of dependence [6]. The CeA causes incorporation of anxiety and fear related information. it is also responsible for reward-related actions. These behaviours are modulated by Dopamine 2 Receptors (D2Rs) located in the CeA [1].
BNST: A constituent of extended amygdala the BNST controls various physiological functions such as anxiety, goal-directed behaviours, feeding behaviour, fear formation. The interaction between the stress, anxiety, and reward systems are mediated by the Central Amygdala projections to the BNST [1].
D2R (Dopamine 2 Receptor): CeL the lateral nucleus of the CeA and capsular nucleus of the CeA has the D2R-expressing neurons. D2R mediates the signalling in CeA which influences the VTA and BNST. The Impulsive behaviour is controlled by D2R-expressing neurons of the CeA → BNST pathway. The mechanism underlying impulsivity is the dysfunctional dopaminergic neurotransmission, in D2R. Impulsive behaviors are controlled by the dopaminergic signalling in the CeA which is the central neural locus that acts via D2R-positive neurons that projects from the CeA to the BNST [1].
Conclusion
The important point of convergence for the neuroadaptation behaviours is the synaptic transmission and the special neuronal circuitry in the CeA-BNST. Research in this fundamental system (CeA) is the goal for therapeutic testing for impulsivity and addiction can be projected by effects of drugs on synaptic transmission. Comprehensive clinical trials are mandatory to explicate the mechanism of CeA-BNST circuitry regulating the impulsivity. This will form the foundation for therapeutic interventions targeted over addiction and impulsivity allied neuropsychiatric disorders.
For more Lupine Publishers Open Access Journals Please visit our
website:
https://lupinepublishers.us/
For more Open Access Journal of Neurology & Neurosurgery articles Please Click Here:
https://lupinepublishers.com/neurology-brain-disorders-journal/Lupine Publishers: Lupine Publishers | Color Changes of Pediatric Den...
Thursday, November 19, 2020
Lupine Publishers: Lupine Publishers | An Actual Statistical Problem ...
Wednesday, November 18, 2020
Lupine Publishers: Lupine Publishers | Evaluation of Combinatorial Ca...
Tuesday, November 17, 2020
Lupine Publishers: Lupine Publishers | Intervarietal Hybridization an...
Monday, November 16, 2020
Lupine Publishers: Lupine Publishers | Perceived Effects of Resource-...
Friday, November 13, 2020
Lupine Publishers: Lupine Publishers | Dimethyl ether as Zero Emissio...
Thursday, November 12, 2020
Lupine Publishers: Lupine Publishers | Evaluation of Ear, Nose and Th...
Wednesday, November 11, 2020
Lupine Publishers: Lupine Publishers | Biogas and Dimethyl Ether are ...
Tuesday, November 10, 2020
Lupine Publishers: Lupine Publishers| About the Influence of Evaporat...
Monday, November 9, 2020
Lupine Publishers: Lupine Publishers | Management of Perinatal and In...
Friday, November 6, 2020
Lupine Publishers| Impact of the Publication of Chinese Treatment Guideline on the Initial Therapy in Parkinson’s Disease in Beijing
Lupine Publishers| Impact of the Publication of Chinese Treatment Guideline on the Initial Therapy in Parkinson’s Disease in Beijing
Abstract
Background: The Guideline for Management of Parkinson’s Disease in China was published in 2006 to standardize Parkinson’s disease treatment. Our objective was to compare the initial PD treatment and their accordance with the recommendations before and after the guideline publication.
Methods: We identified 136 PD patients as part of a hospital-based study in Beijing, and compared the prescriptions of Dopamine Agonists (DA) and levodopa (LD) as initial therapy to evaluate the impact of the publication of Chinese guideline on the therapy of PD.
Results: We found that the publication of the guideline resulted in no difference in initial treatment of PD patients > 65 years. In patients < 65 years, the prescription of DA was significantly increased after the publication of the guideline. There were no significant differences in initial treatment between patients treated in hospitals of different levels or patients with different types of insurance.
Conclusion: The guideline promoted DA utilization as initial treatment in young patients.
Keywords: Parkinson Disease; Initial Therapy; Treatment Guideline; Dopamine Agonist; Beijing
Introduction
The most commonly used antiparkinsonian drugs in China include: anticholinergics (trihexyphenidyl), Amantadine, Levodopa (LD), Dopamine Agonists (DA), Monoamine Oxidase (MAO)-B inhibitors, Catechol-O-Methyltransferase (COMT) inhibitors. LD is the most effective antiparkinsonian drug [1], but its long-term use is associated with motor complications [2]. DA poses less risk of long-term motor complications than LD [3] but is less effective. The challenge during initial PD stages is to control motor symptoms and restore quality of life without increasing the risk of long-term complications. In July 2006, the Guideline for Management of Parkinson’s Disease in China was published. Our objective was to compare the initial PD treatment and their accordance with the recommendations before and after the guideline’s publication.
Subjects and Methods
Participants
One hundred and thirty-six PD patients were enrolled from two hospitals through out-patient department of neurology: Beijing Hospital of the Ministry of Health (class 3-A hospital) and Pinggu traditional Chinese medical hospital (class 2-A hospital). Patients were examined by movement disorders specialists and inquired about the date of symptoms onset, initial treatment, and age at treatment initiation. They were invited to provide all their PD drug prescriptions. Diagnosis was established using standardized criteria [4]. All subjects had at least one prescription of LD, COMT inhibitor (entacapone), Amantadine, anticholinergics (trihexyphenidyl), DA (pramipexole and piribedil), or MAO-B inhibitors (selegiline and rasagiline). Additional inclusion criteria were: disease duration>1 month and Hoehn-Yahr stage less than II.
Chinese Guideline on the Therapy of Pd
The guideline on PD treatment in China was proposed by the Chinese Movement Disorders and Parkinson’s Disease Society. The experts in the study group are all well-recognized on treating PD and related motor disorders. The guideline is a result of a comprehensive review of existing literature and the actual situation in China. The first edition was published in June 2006 in Chinese Journal of Neurology which aimed at making recommendations regarding PD diagnosis and treatment and is widely accessed by both clinical physicians and scientific researchers [5]. The published guideline includes the time of drug utilization and the choice of initial medications in the treatment of early symptoms of Parkinson’s disease. And it was the first time in China to recommend standard Parkinson’s disease treatment. The guideline suggests that DA is the mainstay choice followed by selegiline with or without vitamin E for patients younger than age 65 years without cognitive impairment. When the medications mentioned above fail to improve the symptoms, a combination therapy with compound LD and COMT inhibitor is required. However, for some patients with diminished cognitive function or needing remarkable improvement, compound LD can be the initial therapy. For old (≥65 years) patients, compound LD should be the initial choice, if needed, it can be combined with DA, MAO-B inhibitor or COMT inhibitor. In 2001, America published the third edition of the guidelines for the treatment of PD [6] with detailed description of initial medication on early PD patients. In general, Chinese guideline is similar to the American guidelines except for a few minor aspects. The age divide for DA and LD as initial therapy in China is defined as 65 years while in America it is 70 years old.
Statistical Analysis
We compared the initial therapy and current drug utilization of the 136 PD patients. To estimate the effect of guideline on physicians’ prescription, chi-square test was employed to compare the use of DA and LD as initial therapy. Given delayed effect of the guideline on physicians, January 2007 and January 2010 were defined as two-time dividing points. And patients’ age divide was 65 years old. We compared the two age groups’ use of DA and LD pre-2007, during 2007-2009 and after 2009 as initial treatment. In addition, we also compared the use of DA and LD between class 3-A hospitals and non-class 3-A hospitals by chi-square test. Furthermore, because non-ergot DA was much more expensive than LD, the impact of insurance policy on the use of DA and LD was studied. Non-ergot DA was covered by medical insurance since July 2011. Then we compared the prescription of non-ergot DA before and after 2011 by chi-square test. If the requirements for chi square tests were not met, then Fisher’s exact test was performed. All analyses were performed with SPSS (version 17.0).
Results
This study cohort consisted of 136 patients including 75 males and 61 females. The mean age was 69.68 years. Disease onset ranged from 32 to 84 years old with the mean age of 62.01 years old. Disease duration varied from 1-34 years with the mean length of 7.59 years. The mean value of Hoehn-Yahr stage at PD onset was 1.20. When the study was conducted, Hoehn-Yahr stage ranged from 1-5 with mean value of 2.09. Of all the patients, 22 (16.2%) paid the medical expenses themselves, 84 (61.8%) benefited from medical insurance reimbursement with average costs of RMB 318 per month, the remaining 30 (22.0%) patients enjoyed public health service.
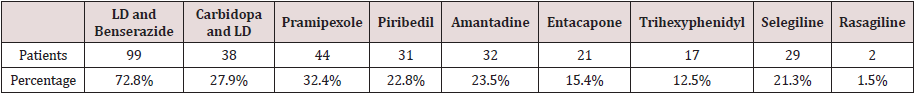
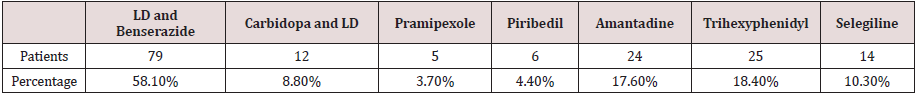
Prevalence of Anti-Parkinsonism Drug (Apd) Use
There was a relatively high proportion of APD users received LD and Benserazide. Among the 136 studied patients, 99 (72.8%) patients used LD and Benserazide, 38 (27.9%) received Carbidopa and LD, 44 (32.4%) received pramipexole, 31 (22.8%) received piribedil, 32 (23.5%) took amantadine, 21 (15.4%) took entacapone, 17 (12.5%) took trihexyphenidyl, 29 (21.3%) received selegiline, and 2 (1.5%) received Rasagiline. A total of 116 (85.3%) received at least one LD (LD and Benserazide or Carbidopa and LD) while 55.9% of the studied patients received DA (pramipexole or piribedil). In Table 1, prescriptions for each medication are presented. Prevalence of initial prescription is as follows (Table 2): 58.1% (79) received LD and Benserazide, ranking first among APD; 8.8% (12/136) received Carbidopa and LD, 3.7% (5/136) received pramipexole, 4.4% (6/136) received piribedil, 17.6% (24/136) took amantadine, 18.4% (23/136) received trihexyphenidyl, and 10.3% (14/136) received selegiline. LD was chosen as initial therapy by a total of 91 (66.9%) patients, while only 11 (8.1%) preferred DA as initial prescription.
Effects of Publishing the Guideline on the Prescription Choice
Table 3 summarizes the changes of LD and DA prescriptions before and after the guideline publication. No significant difference between LD and DA prescriptions was found among patients > 65 years old before and after 2007 (P=0.290). In patients < 65 years, initial therapy of LD and DA differed before 2007, during 2007- 2009 and after 2009 (P=0.005). 4.2% patients received DA as initial therapy before 2007, and the proportion significantly increased to 42.9% during 2010-2012 (P=0.028). However, no significance was found between pre-2007 and 2007-2009.
Table 3: DA and LD used as initial prescriptions before and after the publication of the guideline
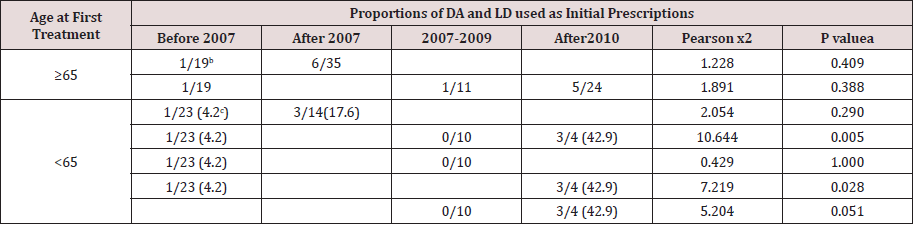
a) Comparison of the number of patients used DA and LD as initial prescriptions at different time-periods using chi-square test or the Fisher’s exact test with one degree of freedom where applicable. Time periods including < 2007 and > 2007 or < 2007, 2007-2009 and >2009.
b) Proportions of DA and LD utilization.
c) Percentage of DA utilization.
The Influence of Hospital Class and Insurance Types on Initial Prescriptions
Initial therapy of LD and DA were compared between Class3-A hospitals and non-Class3-A hospitals. A total of 104 patients were enrolled. 88 patients received initial prescription in Class-3A hospital among whom 76 received LD and 12 used DA. There were 16 patients receiving initial prescription in non-Class 3-A hospitals, among whom 15 received LD and 1 received DA. Initial prescription of DA was not significantly different between Class 3-A hospitals (13.6%) and non-Class 3-A hospitals (6.3%) (P=0.686).
Changes of Non-Ergot Da Prescription Before and After it was Covered by Medical Insurance
It was not until 1/7/2011 that non-ergot DA (pramipexole and piribedil) were formally covered by medical insurance in Beijing. Among the 111 patients in our study before July 2011, 50 (45%) patients received non-ergot DA (28 received pramipexole and 22 received piribedil). From the start of the survey to April 2012, the number of patients receiving non-ergot DA increased to 76 (44 received pramipexole and 32 received piribedil) with a proportion up to 55.9%. However, no significant insurance-related differences were found.
Discussion
Impact of the Publication of the Guideline on Initial Prescription
In our study, the guideline did not significantly influence initial prescription in patients ≥ 65 years old. The outcomes were under expectation since the chances of motor complication induced by LD remained relatively uncommon in old patients. The suggestion of LD prescription in patients ≥ 65 years in the guideline was in line with medical practice before. The guideline dramatically promoted DA utilization in young patients. In general, this statistic results were in agreement with the population-based study in France [7]. However, there existed delay in the implementation of the guideline because no significant differences were found between pre-2007 and 2007-2009. However, initial prescription differed significantly between pre-2007 and 2010-2012. The delay in the practice of guideline could be due to the lack of Chinese physicians’ attention initially. Economy and medical insurance also may have influence on drug prescription. Increased influence of the guideline on Chinese physicians’ practice since 2010 was mainly driven by Movement disorders and Parkinson’s disease study group of Chinese Society of Neurology. Besides, the study group revised and republished the guideline in 2009 which may further enhance the influence of the guideline. It is likely that other factors such as insurance coverage, the publication of related clinical trials and the promotion of pharmaceutical manufactures also contribute to the phenomenon. The guideline improved the proportion of DA utilization in young patients. However, according to our study, a large number of patients < 65 years received LD initially with a proportion of 63.9%, while only 13.7% patients received DA as the initial therapy. This is consistent with surveys abroad [8-11]. It implied that only a minority of physicians prescribed APD based on the guideline and it took time to change clinical practice after the publication of the guideline.
The Influence of Hospital Level and Medical Insurance on Initial Prescription
No significant influence of hospital level and the types of medical insurance on initial prescription were found. Possible reasons were as follows: first of all, daily clinical practice is compliant with the principle of PD medication, both physicians and patients aimed at controlling symptom. Secondly, most patients from class 2-A hospitals we surveyed were from Pinggu traditional Chinese medical hospital where regulatory outpatient service was offered by the physicians from Beijing Hospital of the Ministry of Health. The offered outpatient service can largely improve diagnostic and treatment level. However, some other class 2-A hospitals may offer poor service and patients from those hospitals may not be included in our study. Among the 20 patients who were free of medical insurance, 10 patients were from other provinces. However, these 10 patients had the ability to afford medical costs and had high drug compliance. Finally, another limitation of the presented study should be taken into account since our findings were based on a relatively small number of subjects. Especially, the proportions of initial prescriptions from class 2-A hospitals and patients free of medical insurance were quite small. Two DA (pramipexole and piribedil) started to be covered by medical insurance since 1/7/2011 in Beijing which drove DA utilization modestly (P=0.098). We then performed Fisher exact test with a p value of 0.058. Significant difference may be found when a large number of patients are enrolled. To some extend our study shows that drug compliance and economic burden are needed to be taken into consideration when physicians prescribe medications in China. Moreover, the guideline promotion needs to be supported by medical insurance to some extent.
For more Lupine Publishers Open Access Journals Please visit our
website:
https://lupinepublishers.us/
For more Open Access Journal of Neurology & Neurosurgery articles Please Click Here:
https://lupinepublishers.com/neurology-brain-disorders-journal/
Lupine Publishers| Depression and Anxiety Frequency in Patients Hospitalized on the Guadalajara Regional Military Hospital in the Month of April 2019
Lupine Publishers| Journal of Neurology and Brain Disorders Abstract Observe and Identify patients that presented depression ...

-
Lupine Publishers| Journal of Neurology and Brain Disorders Abstract Recent research suggests that schizophrenia is associated with the ...
-
Lupine Publishers| Journal of Neurology and Brain Disorders Abstract Observe and Identify patients that presented depression ...
-
Lupine publishers LLC | Lupine Publishers Review 1. Lupine Publishers LLC isa world’s leading Online Publishin...