Wednesday, August 28, 2019
Lupine Publishers: Soil Texture of Nesting Sites and Breeding Populat...
Lupine Publishers: Soil Texture of Nesting Sites and Breeding Populat...: Lupine Publishers- Environmental and Soil Science Abstract Investigating the breeding population and soil texture of breeding ...
Lupine Publishers: Change of Evaporations Leads to Climate Change
Lupine Publishers: Change of Evaporations Leads to Climate Change: Lupine Publishers- Environmental and Soil Science Short Communication The basis of all floods and droughts is water, its e...
Monday, August 26, 2019
Lupine Publishers: Lupine Publishers| Some Aspects of Red Special Win...
Lupine Publishers: Lupine Publishers| Some Aspects of Red Special Win...: Lupine Publishers- Environmental and Soil Science Abstract Due to increasing environmental radionuclide background, the scien...
Saturday, August 24, 2019
Lupine Publishers: Lupine Publishers | Gastrointestinal Parasites Fou...
Lupine Publishers: Lupine Publishers | Gastrointestinal Parasites Fou...: Lupine Publishers | Journal of Veterinary Science Abstract This paper is the first part of a three (3) part series of review...
Friday, August 23, 2019
Lupine Publishers: Lupine Publihsers | The Development Fortified Pan ...
Lupine Publishers: Lupine Publihsers | The Development Fortified Pan ...: Lupine Publishers | Journal of Veterinary Science Abstract The main objective of the research is to develop pan bread nutri...
Thursday, August 22, 2019
Prevalence of Organic Mental Disorders in a General Hospital in Izhevsk, Russia| Lupine Publishers
Journal of Neurology & Neurosurgery- Lupine Publishers
Abstract
Methods: The subjects (323 patients aged from 18 to 59 years) were selected using the method of continuous sampling. All subjects were asked to answer the questions from the Russian version of the Brief International Neuropsychiatric Questionnaire (MINI 5.0.0.).
Results: The prevalence of OMD was 55.1%. OMD were more common in older patients (50-59 years) and in patients with chronic somatic diseases. 36.5% of patients with OMD were diagnosed with pre-dementia. The comorbidity of OMD with other mental disorders was statistically significant for depression and anxiety disorders.
Conclusion: Knowledge of OMD risk factors can contribute to early detection and adequate treatment of OMD in patients of general hospitals.
Keywords: Organic mental disorders; Prevalence; risk factors; General hospital
Background and objectives
Researchers emphasize that early, even immediate detection of organic mental disorders is extremely important [6]. At the moment, studies of organic mental disorders (OMD) in in-patients of therapeutic units in Udmurtia are limited. The paper’s objective was to study the prevalence and risk factors of OMD in medical patients and identify correlative factors.
Methods
The subjects were selected using the method of continuous sampling. The group included every patient aged 18 to 59 referred to the hospital unit number 1. The average length of hospitalization per patient was 18.3 days. A total of 352 patients were selected for the study. 29 of them (11 men and 18 women) were not included in the study for various reasons (refusal, severe somatic condition, etc.). Consequently, the study sample consisted of 323 patients, including 147 (45.5%) men and 176 (54.5%) women. Ethnic background of the study population: 214 (66.3%) Russians, 77 (23.8) Udmurts and 32 (9.9%) other. All participants were divided into the following age groups: 18-39 years– 37%, 40-49 years– 31% and 50-59 years– 32%. 71.5% of the study population were hospitalized due to exacerbation of a chronic somatic disease and 28.5% – due to an acute somatic disease.
All subjects were asked to answer the questions from the Russian version of the Brief International Neuropsychiatric Questionnaire (MINI 5.0.0.) [15]. Additionally, the survey used the diagnostic criteria of ICD-10 for organic mental disorders and the criteria for tobacco addiction. MINI is a standardized diagnostic interview for major mental disorders according to DSM-IV and ICD-10. The reliability and validity of MINI correspond to SCID-P and CIDI, but an important advantage of MINI is that interviewing requires less time.
Information on somatic diagnoses, psychiatric consultations and prescribed psychotropic medications was obtained from medical records (medical history, patient records). Socio-demographic questions (gender, age, marital status, ethnic background, education and occupation) are part of MINI. Participation in the study was voluntary; the patients were informed of their right to refuse to participate. In case of consent, complete anonymity was guaranteed. The patients have signed a written ‘Informed Consent’.
Questioning and interviewing in each case were conducted during the first 72 hours of hospitalization. The diagnostic survey was conducted by three medical doctors who had been trained to use MINI at the Department of Psychiatry of Izhevsk State Medical Academy. The STATISTICA 5.0 software was used to analyze the data. The following tests were used: the t-test to compare average values (average monthly income, average age, etc.) and the chisquare test to assess qualitative characteristics (gender, ethnic background, social status, etc.). To analyze comorbidity, the software Epi Info, Version 6 [16] was used. The OMD comorbidity was determined as follows: the probability index of concomitant disease in the population with OMD was divided by the probability index of concomitant disease in the population without OMD. The manuscript has been assessed by the Ethics Committee (Institutional Board Review) in the Izhevsk State Medical Academy.
Results
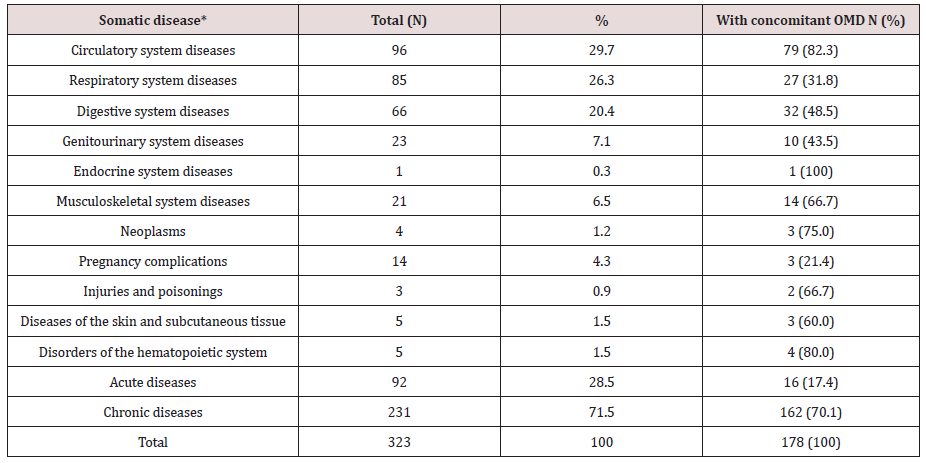
* In case of concomitant somatic diseases, only the principle diagnosis was considered.
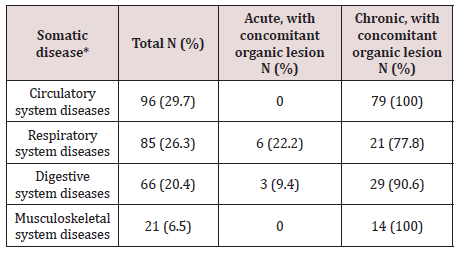
Acute diseases predominated in the group of patients with respiratory system disorders – 58.8%, and disorders of other organs and systems were mainly represented by chronic diseases (genitourinary system– 78.3%, digestive system– 78.8%, cardiovascular– 94.8%, and musculoskeletal– 100%). Acute diseases were more often diagnosed in patients aged 18-39 (55.8%), while chronic forms predominated in the age groups of 40-49 and 50-59 years – 77.2% and 98.0% respectively. OMD were more often diagnosed in patients with chronic somatic diseases, especially those with diseases of the circulatory and musculoskeletal systems – 100% of the cases (Table 2).
The OMD prevalence in the sample was 55.1% (178 cases). The average age of the respondents with OMD was 46.6 years (Std. Dev. = 10.2). The average OMD duration was 6.4 years, with the minimum less than one year and the maximum of 45 years (Std. Dev. = 6.4).
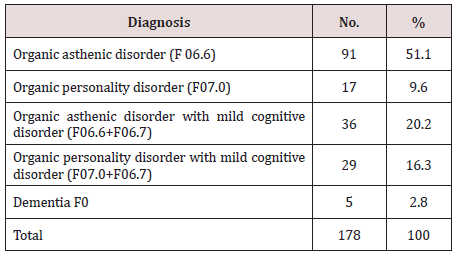
B. The Breakdown of OMD is Given Below (Table 3):
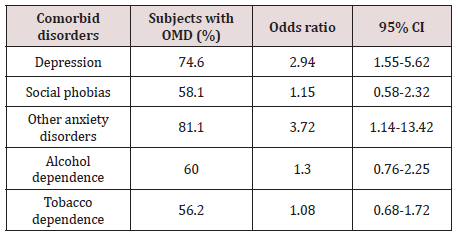
In terms of socio-demographic factors, a reliable correlation with the age of the patients was identified: OMD in the age groups of 18-39, 40-49 and 50-59 years were diagnosed in 19.7%, 33.2% and 47.2% of the cases respectively (P = 0.000). There was no statistically significant correlation between OMD and ethnic background, marital status, education or social status. The tendency to a greater predisposition to OMD in women (56.7% versus 43.3% in men) was identified. There were other psychiatric disorders diagnosed in the sample: depressive disorders – 20.7%, alcohol dependence–24.8%, tobacco dependence – 45.2%, social phobias – 13.3%, other anxiety disorders - 6.5% (ICD-10 codes: F40.01, F41.0, F41.1, F42.8). The comorbidity of OMD with other mental disorders was statistically significant for depression and anxiety disorders (Table 4). 20.2% of patients with OMD were counseled by a psychiatrist.Discussion and Conclusion
The researchers emphasize it is not a somatic pathology but its severity and duration that play a role in the development of OMD. Apparently this is why OMD were statistically more often diagnosed in patients with chronic rather than acute somatic diseases (70.1% vs 17.4%). Moreover, 100% of the respondents with diseases of the circulatory or musculoskeletal systems were diagnosed with OMD. High occurrence of OMD was observed among patients with diseases of the digestive and respiratory systems – 90.6% and 77.8% respectively.
There was no correlation between OMD and such sociodemographic factors as gender, ethnicity, marital status, education or social status. There was a reliable correlation between OMD and the age of the patients, probably because of the greater occurrence of chronic somatic diseases and accumulation of cerebrovascular diseases in elderly patients [4]. Thus, the epidemiological indicators of OMD in the general hospital were extremely high, especially among patients with chronic diseases. One third of patients with OMD were diagnosed with mild cognitive impairment, and according to medical sources, there is a high risk that this condition may transform into dementia in the next few years.
Such results may indicate insufficient diagnostics and lack of OMD treatment. The reasons for the under-diagnosis may be insufficient psychiatric care in hospitals and lack of awareness among therapists of the OMD clinical picture. Awareness of epidemiology and risk factors can contribute to early detection and treatment of OMD. Identification and appropriate treatment of OMD is an extremely important task due to the unfavorable prognosis.
For more LupinePublishers Open Access Journals Please visit our website:
https://lupinepublishers.us/
https://lupinepublishers.us/
For more Open Access Journal of Neurology & Neurosurgery articles
Please Click Here:
https://lupinepublishers.com/neurology-brain-disorders-journal/
https://lupinepublishers.com/neurology-brain-disorders-journal/
To
Know More About OpenAccess Publishers Please Click on Lupine Publishers
Lupine Publishers: Lupine Publishers | Use of Dietary Yeast and its P...
Lupine Publishers: Lupine Publishers | Use of Dietary Yeast and its P...: Lupine Publishers | Journal of Veterinary Science Abstract All around the world, sheeps and goats play an important role in...
Tuesday, August 20, 2019
Lupine Publishers: Bowels and Urine Odors and Its Solutions | Lupine ...
Lupine Publishers: Bowels and Urine Odors and Its Solutions | Lupine ...: Journal of Diabetes and Obesity | Lupine Publishers Opinion From the beginning time people go for bowel outside in the fi...
Friday, August 16, 2019
Isolated and Recurrent Peripheral Facial Palsy Revealing Primary Sjogren’s Syndrome
Journal of Neurology & Neurosurgery- Lupine Publishers
Abstract
Keywords: Peripheral facial palsy; Primary Sjögren’s syndrome; Facial paralysis; Neuro Sjogren
Introduction
<The spectrum of PSS-associated neurological manifestations may include: multiple mononeuropathy, symmetrical axonal sensorimotor polyneuropathy, sensory ataxic neuropathy, painful sensory neuropathy, cranial neuropathy, autonomic neuropathy, radiculoneuropathy, aseptic meningitis, encephalopathy, psychiatric symptoms, chorea, seizures, chronic myelopathies, multiple sclerosis-like syndrome, and cognitive impairment [5-8]. Neurological involvement may be the first manifestation of PSS in approximately 25% of cases [7]. Of all the possible neurological manifestations of PSS, peripheral facial palsy (PFP) remains exceptional and unusual [9], and only a few sporadic cases were reported in the medical literature [9-12]; these inaugural forms of the disease represent a real diagnostic challenge for clinicians. We report an original observation of isolated and recurrent PFP as inaugural symptom of PSS.
Case Report
In somatic examination, the patient was apyretic, with correct conscious, respiratory, and hemodynamic status. We noted a marked dryness of the skin and the tongue.
Laboratory tests revealed a marked biological inflammatory syndrome with erythrocyte sedimentation rate at 68 mm/H1, C-reactive protein at 18 mg/l, and polyclonal hypergammaglobulinemia at 24.6 mmol/l. the other basic tests were within normal limits: blood count, creatinine, serum calcium, ionogram, fasting glucose, transaminases, muscle enzymes, lipid parameters, and thyroid hormones. Immunological exploration showed positive anti-nuclear autoantibodies at 1/640 with positive anti-SSA antibodies at 50 IU. The specialized ophthalmologic examination objectified xerophthalmia with bilateral filamentous keratitis and a positive Schirmer’s test.
Biopsy of the accessory salivary glands showed a stage 3 chronic sialadenitis according to the Chisholm classification. Thus, the diagnosis of PSS was retained based on the following criteria: xerophthalmia, xerostomia, positive ophthalmological tests, stage 3 chronic sialadenitis, and positive anti-nuclear and anti-SSA antibodies. Cerebrospinal fluid analysis and cerebromedullary MRI did not show signs suggestive of specific neurological involvement of PSS (neuro-Sjögren). Similarly, other systemic complications of PSS and a possible lymphomatous transformation were eliminated by specific investigations. At the end of this assessment, the diagnosis of a recurrent and isolated PFP revealing PSS was retained. The patient was treated with systemic corticosteroid therapy at a dose of 1 mg/kg/day and hydroxychloroquine at a dose of 400 mg/d, salicylic acid at a dose of 100 mg/d, and symptomatic treatment of xerophthalmia and xerostomia, with favorable evolution. No recurrence of the PFP has been noted for five years now.
Discussion
These forms of isolated and SSP-revealing cranial neuropathies are often ignored and neglected by clinicians, and thus sometimes responsible for a very important diagnosis delay [16]. The exact pathophysiology of this neuropathy is not very well known. It appears to be multifactorial involving vasculitis, autoimmunity, inflammation, and cryoglobulinemia [4,5]. A reported case of PSSassociated PFP involved, in addition to these classic pathogenic factors, a vitamin B12 deficiency [11]. Finally, it should be kept in mind that a PFP for rapid onset and/or progression during PSS should raise concerns about the lymphomatous transformation of this disease [17].
Conclusion
For more LupinePublishers Open Access Journals Please visit our website:
For more Open Access Journal of Neurology & Neurosurgery articles
Please Click Here:
https://lupinepublishers.com/neurology-brain-disorders-journal/
https://lupinepublishers.com/neurology-brain-disorders-journal/
To
Know More About OpenAccess Publishers Please Click on Lupine Publishers
Monday, August 12, 2019
Lupine Publishers: The Physical Study of Vertical Structure of Temper...
Lupine Publishers: The Physical Study of Vertical Structure of Temper...: Journal of Oceanography | Lupine Publishers Abstract Always oceanographers pay attention to layer structure in the sea environme...
Saturday, August 10, 2019
Lupine Publishers: Lupine Publishers | Anti-Synepthelichorial Placent...
Lupine Publishers: Lupine Publishers | Anti-Synepthelichorial Placent...: Lupine Publishers | Journal of Veterinary Science Hens were immunized with a macerate of goat and sheep placentomes. Immunizations w...
Friday, August 2, 2019
Lupine Publishers: Lupine Publishers | Molecular Typing Of Capsular P...
Lupine Publishers: Lupine Publishers | Molecular Typing Of Capsular P...: Lupine Publishers | Journal of Veterinary Science Abstract Forty five Staphylococcus aureus isolated from cases of bovin...
Thursday, August 1, 2019
Lupine Publishers: Lupine Publishers | Survey on Pathological Lesion ...
Lupine Publishers: Lupine Publishers | Survey on Pathological Lesion ...: Lupine Publishers | Journal of Veterinary Science Abstract A cross-sectional study was conducted from October 2016 to July...
Subscribe to:
Posts (Atom)
Lupine Publishers| Depression and Anxiety Frequency in Patients Hospitalized on the Guadalajara Regional Military Hospital in the Month of April 2019
Lupine Publishers| Journal of Neurology and Brain Disorders Abstract Observe and Identify patients that presented depression ...

-
Greetings from OJNBD!! Wishing you a harvest of blessings, good health and good times. Happy Thanksgiving day !
-
Lupine Publishers| Journal of Neurology and Brain Disorders Abstract Observe and Identify patients that presented depression ...
-
Lupine Publishers| Journal of Neurology and Brain Disorders Abstract Recent research suggests that schizophrenia is associated with the ...