Journal of Neurology & Neurosurgery- Lupine Publishers
Abstract
Methods: The subjects (323 patients aged from 18 to 59 years) were selected using the method of continuous sampling. All subjects were asked to answer the questions from the Russian version of the Brief International Neuropsychiatric Questionnaire (MINI 5.0.0.).
Results: The prevalence of OMD was 55.1%. OMD were more common in older patients (50-59 years) and in patients with chronic somatic diseases. 36.5% of patients with OMD were diagnosed with pre-dementia. The comorbidity of OMD with other mental disorders was statistically significant for depression and anxiety disorders.
Conclusion: Knowledge of OMD risk factors can contribute to early detection and adequate treatment of OMD in patients of general hospitals.
Keywords: Organic mental disorders; Prevalence; risk factors; General hospital
Background and objectives
Researchers emphasize that early, even immediate detection of organic mental disorders is extremely important [6]. At the moment, studies of organic mental disorders (OMD) in in-patients of therapeutic units in Udmurtia are limited. The paper’s objective was to study the prevalence and risk factors of OMD in medical patients and identify correlative factors.
Methods
The subjects were selected using the method of continuous sampling. The group included every patient aged 18 to 59 referred to the hospital unit number 1. The average length of hospitalization per patient was 18.3 days. A total of 352 patients were selected for the study. 29 of them (11 men and 18 women) were not included in the study for various reasons (refusal, severe somatic condition, etc.). Consequently, the study sample consisted of 323 patients, including 147 (45.5%) men and 176 (54.5%) women. Ethnic background of the study population: 214 (66.3%) Russians, 77 (23.8) Udmurts and 32 (9.9%) other. All participants were divided into the following age groups: 18-39 years– 37%, 40-49 years– 31% and 50-59 years– 32%. 71.5% of the study population were hospitalized due to exacerbation of a chronic somatic disease and 28.5% – due to an acute somatic disease.
All subjects were asked to answer the questions from the Russian version of the Brief International Neuropsychiatric Questionnaire (MINI 5.0.0.) [15]. Additionally, the survey used the diagnostic criteria of ICD-10 for organic mental disorders and the criteria for tobacco addiction. MINI is a standardized diagnostic interview for major mental disorders according to DSM-IV and ICD-10. The reliability and validity of MINI correspond to SCID-P and CIDI, but an important advantage of MINI is that interviewing requires less time.
Information on somatic diagnoses, psychiatric consultations and prescribed psychotropic medications was obtained from medical records (medical history, patient records). Socio-demographic questions (gender, age, marital status, ethnic background, education and occupation) are part of MINI. Participation in the study was voluntary; the patients were informed of their right to refuse to participate. In case of consent, complete anonymity was guaranteed. The patients have signed a written ‘Informed Consent’.
Questioning and interviewing in each case were conducted during the first 72 hours of hospitalization. The diagnostic survey was conducted by three medical doctors who had been trained to use MINI at the Department of Psychiatry of Izhevsk State Medical Academy. The STATISTICA 5.0 software was used to analyze the data. The following tests were used: the t-test to compare average values (average monthly income, average age, etc.) and the chisquare test to assess qualitative characteristics (gender, ethnic background, social status, etc.). To analyze comorbidity, the software Epi Info, Version 6 [16] was used. The OMD comorbidity was determined as follows: the probability index of concomitant disease in the population with OMD was divided by the probability index of concomitant disease in the population without OMD. The manuscript has been assessed by the Ethics Committee (Institutional Board Review) in the Izhevsk State Medical Academy.
Results
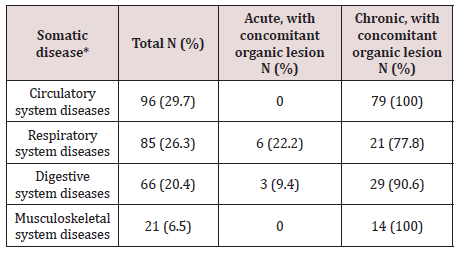
* In case of concomitant somatic diseases, only the principle diagnosis was considered.
Acute diseases predominated in the group of patients with respiratory system disorders – 58.8%, and disorders of other organs and systems were mainly represented by chronic diseases (genitourinary system– 78.3%, digestive system– 78.8%, cardiovascular– 94.8%, and musculoskeletal– 100%). Acute diseases were more often diagnosed in patients aged 18-39 (55.8%), while chronic forms predominated in the age groups of 40-49 and 50-59 years – 77.2% and 98.0% respectively. OMD were more often diagnosed in patients with chronic somatic diseases, especially those with diseases of the circulatory and musculoskeletal systems – 100% of the cases (Table 2).
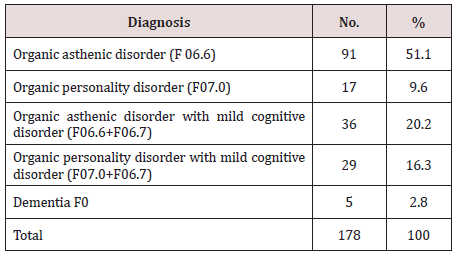
The OMD prevalence in the sample was 55.1% (178 cases). The average age of the respondents with OMD was 46.6 years (Std. Dev. = 10.2). The average OMD duration was 6.4 years, with the minimum less than one year and the maximum of 45 years (Std. Dev. = 6.4).
B. The Breakdown of OMD is Given Below (Table 3):
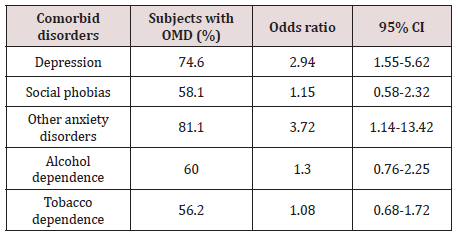
In terms of socio-demographic factors, a reliable correlation with the age of the patients was identified: OMD in the age groups of 18-39, 40-49 and 50-59 years were diagnosed in 19.7%, 33.2% and 47.2% of the cases respectively (P = 0.000). There was no statistically significant correlation between OMD and ethnic background, marital status, education or social status. The tendency to a greater predisposition to OMD in women (56.7% versus 43.3% in men) was identified. There were other psychiatric disorders diagnosed in the sample: depressive disorders – 20.7%, alcohol dependence–24.8%, tobacco dependence – 45.2%, social phobias – 13.3%, other anxiety disorders - 6.5% (ICD-10 codes: F40.01, F41.0, F41.1, F42.8). The comorbidity of OMD with other mental disorders was statistically significant for depression and anxiety disorders (Table 4). 20.2% of patients with OMD were counseled by a psychiatrist.Discussion and Conclusion
The researchers emphasize it is not a somatic pathology but its severity and duration that play a role in the development of OMD. Apparently this is why OMD were statistically more often diagnosed in patients with chronic rather than acute somatic diseases (70.1% vs 17.4%). Moreover, 100% of the respondents with diseases of the circulatory or musculoskeletal systems were diagnosed with OMD. High occurrence of OMD was observed among patients with diseases of the digestive and respiratory systems – 90.6% and 77.8% respectively.
There was no correlation between OMD and such sociodemographic factors as gender, ethnicity, marital status, education or social status. There was a reliable correlation between OMD and the age of the patients, probably because of the greater occurrence of chronic somatic diseases and accumulation of cerebrovascular diseases in elderly patients [4]. Thus, the epidemiological indicators of OMD in the general hospital were extremely high, especially among patients with chronic diseases. One third of patients with OMD were diagnosed with mild cognitive impairment, and according to medical sources, there is a high risk that this condition may transform into dementia in the next few years.
Such results may indicate insufficient diagnostics and lack of OMD treatment. The reasons for the under-diagnosis may be insufficient psychiatric care in hospitals and lack of awareness among therapists of the OMD clinical picture. Awareness of epidemiology and risk factors can contribute to early detection and treatment of OMD. Identification and appropriate treatment of OMD is an extremely important task due to the unfavorable prognosis.
For more LupinePublishers Open Access Journals Please visit our website:
https://lupinepublishers.us/
https://lupinepublishers.us/
For more Open Access Journal of Neurology & Neurosurgery articles
Please Click Here:
https://lupinepublishers.com/neurology-brain-disorders-journal/
https://lupinepublishers.com/neurology-brain-disorders-journal/
To
Know More About OpenAccess Publishers Please Click on Lupine Publishers






No comments:
Post a Comment